Diabetes is a common disease that affects about 1 out of 10 Americans, according to the American Diabetes Association. As for those aged 65 and older, over 25% are affected by diabetes. Diabetes affects the body’s ability to effectively produce and/or use insulin to control blood sugar (glucose) levels. Too much glucose in the blood can damage many parts of the body, including the eyes.
A few eye diseases can be brought upon by diabetes, including glaucoma, cataracts, and diabetic macular edema. The most common eye disease that leads to vision loss in diabetic adults is diabetic retinopathy.
Diabetic Retinopathy
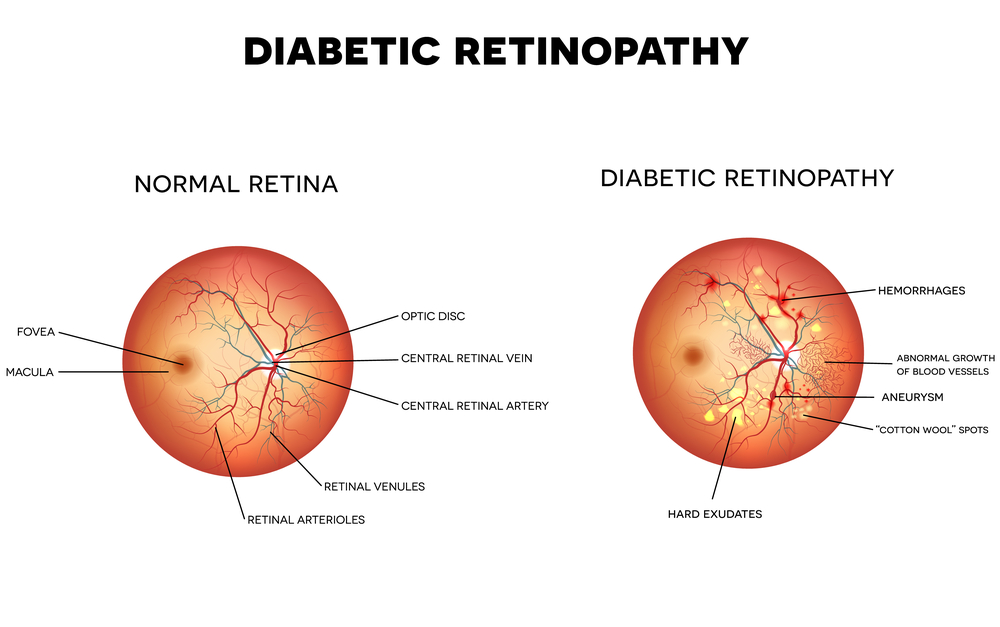
Diabetic retinopathy is an eye disease that is caused by high blood sugar levels, causing blood vessels in the retina to swell, leak, and in some cases, close altogether. In other instances, abnormal blood vessels can also begin to grow on the retina. All of these abnormal changes can cause vision loss. There are four stages of diabetic retinopathy:
- Mild nonproliferative retinopathy: the earliest stage of diabetic retinopathy in which small swellings occur in the retina’s blood vessels.
- Moderate nonproliferative retinopathy: some blood vessels become blocked in the retina at this stage.
- Severe nonproliferative retinopathy: at this stage, the retina’s blood vessels become blocked and lack blood supply, causing blood vessels to develop and grow.
- Proliferative retinopathy: the most advanced stage of diabetic retinopathy in which new blood vessels continue to abnormally develop and grow, leaking blood into the retina and causing severe vision loss.
Symptoms
Symptoms of diabetic retinopathy typically include blurred vision, spots (floaters), trouble seeing colors, and empty or dark areas in the vision. If left untreated, vision loss can occur in the form of proliferative retinopathy and macular edemas (swelling of the macula, caused by abnormal fluid in the retina).
Diagnosis and Treatment
To determine if you have diabetic retinopathy, your ophthalmologist will dilate your pupil to see your retina. Then, they may do an OCT to determine if there is swelling in the macula. They also might do a fluorescein angiography to see if the blood vessels in your retina are blocked or leaking fluid.
Once your ophthalmologist determines what stage you are at, a treatment plan will be put into place. They might suggest laser therapy (photocoagulation), medicinal inhibitors to slow down the effects of diabetic retinopathy, injections, or removing parts of the vitreous (vitrectomy).
Treatment plans will vary based on the stage and severity of diabetic retinopathy. If you are experiencing vision loss, dark spots or “holes” in your vision, floaters, or distorted vision, call our office at 954-772-3337 to schedule a consultation with our retinal specialists. Dr. Burgess, Dr. Lara, and Dr. Villate are highly skilled ophthalmologists with extensive experience treating diabetic retinopathy and other retinal diseases related to diabetes.
